Transforming Health through research
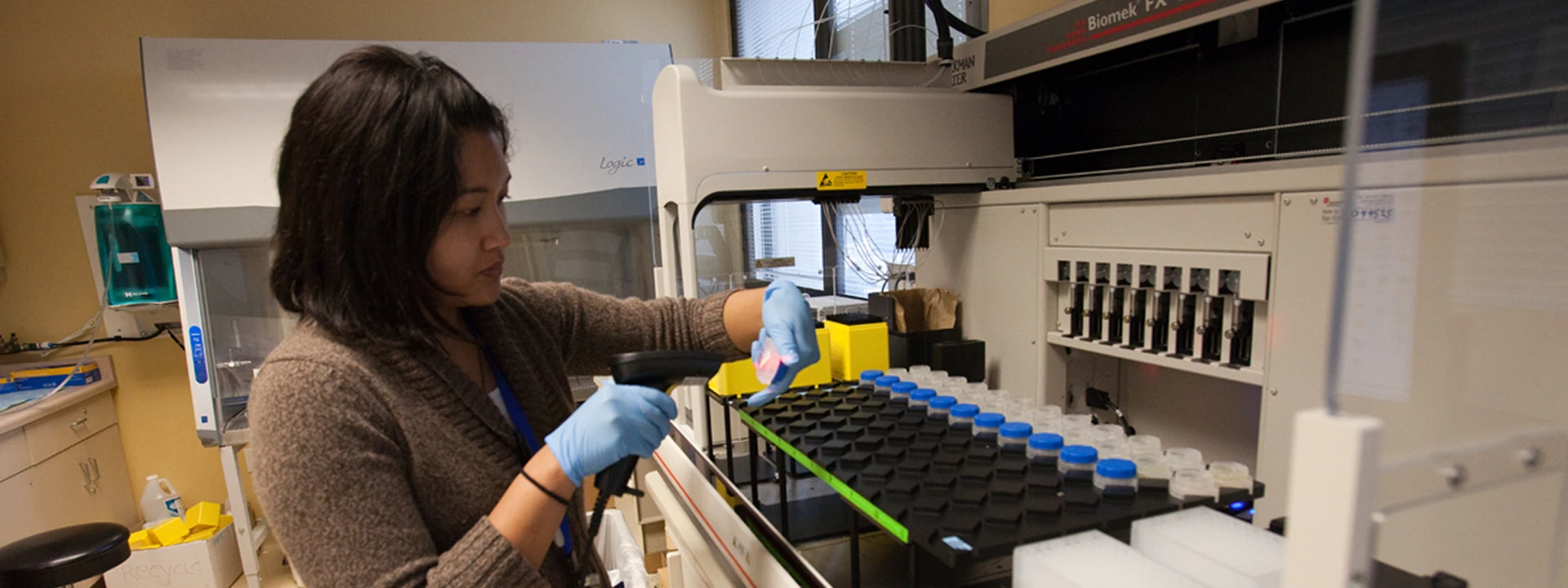
Kaiser Permanente Division of Research
Publications and Studies
Tools for Clinicians and Collaborators
We provide support and direction to clinician researchers and external partners with all aspects of collaborating, planning, and conducting clinical research within Kaiser Permanente Northern California.
Our Scientists
Margae J. Knox , PhD, MPH
Research interests include social determinants of health and new models to improve care delivery.
Read Scientist’s BioParticipate in a Study
Visit the KP Study Search website to find out how participating in research studies benefits participants and society at large, and learn which studies are looking for participants.





