Kaiser Permanente study finds symptoms improved in both a “collaborative care” model and typical psychiatric care
A study comparing traditional psychiatric treatment of depression and anxiety with a team-based collaborative care approach found that patients in both models saw significant improvement of their symptoms, but the improvement was even stronger in the collaborative care approach. The study was published in the Journal of Clinical Psychiatry.
Team-based collaborative care has been offered to Kaiser Permanente Northern California (KPNC) patients since 2020. Care is focused on frequent symptom monitoring and treatment personalized to patient symptoms, with care provided by therapists with support from pharmacists. The study covered a period early in the COVID pandemic when most care was being delivered virtually through telehealth.

Patients in the collaborative care group with depression saw an average 9-point improvement as measured by a 27-point patient health questionnaire, a validated tool that can be used to measure patient depressive symptoms at each visit. There was a 5-point improvement in the traditional care group.
The improvement in both groups was notable, particularly because care took place largely through phone and video visits, said lead author Kathryn Erickson-Ridout, MD, PhD, a psychiatrist with The Permanente Medical Group and adjunct investigator with the Kaiser Permanente Division of Research. “The data shows that in both programs, patients with mild to moderate symptoms improve,” she said. “In fact, a high proportion of depression patients reached full remission of their symptoms in both programs — 27% in specialty care and 43% in collaborative care, when the national average is around 10%.
“The average depression patient in this study moved from moderate symptoms to not meeting criteria for depressive disorder,” Erickson-Ridout added. “That kind of improvement is great to see because depression remission can offer improved functioning and less risk of relapse.”
Erickson-Ridout was also encouraged by what the results suggest about the collaborative care being used by KPNC. Collaborative care is used nationally and features patient-centered care from a team of providers, regular evaluation of patient symptoms and status, and treatment to a symptom target using evidence-based practices. The KPNC version adds monitoring the patient’s progress and recommending any additional interventions into every visit, medication management by program pharmacists, and integration of symptom tracking into existing clinical tools.
“The key part of the model is what we call measurement-based care, meaning that patients are assessed regularly with questionnaires about their symptoms, and the results help the clinician guide next steps of care,” Erickson-Ridout said. “If we engage with patients in a structured way they appear to have better outcomes.”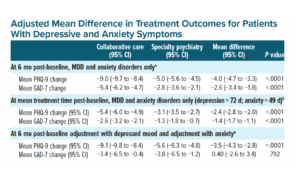
Another benefit of collaborative care, she said, is that therapists and pharmacists assist the psychiatrist in a team approach that can address the national shortage in mental health clinicians.
The study compared 1,607 mild-to-moderate depression patients in collaborative care with 8,773 patients in specialty psychiatry, and 570 mild-to-moderate anxiety patients in collaborative care with 2,365 in specialty psychiatry. Their symptoms were tracked for 6 months between 2020 and 2021.
The collaborative care depression patients saw a 9-point decrease in symptoms as measured on the 27- point Patient Health Questionnaire-9, and collaborative care anxiety patients saw a 5.4-point reduction in symptoms as measured on the 27-point Generalized Anxiety Disorder-7 Scale. For those in specialty psychiatry care, depression symptoms went down 5 points and anxiety symptoms down 2.8 points.

“This initiative exemplifies KPNC’s Behavioral Health service line’s continuous dedication to implementing evidence-based interventions like collaborative care on a larger scale,” said co-author Maria T. Koshy, MD, a psychiatrist with The Permanente Medical Group and director of regional mental health administration. “It also contributes to the expanding body of research supporting multi-disciplinary, team-based psychotherapy and medication management programs, aimed at providing patients with depression swift and significant symptom relief.”
Collaborative care option growing
KPNC patients who seek treatment for mild to moderate depression or anxiety symptoms through their primary care doctor or directly with psychiatry choose either collaborative care or specialty psychiatric care with assistance from their doctor and mental health clinicians.
Specialty psychiatric care involves meeting with a psychiatrist, who develops a treatment plan in partnership with the patient based on their clinical judgment and may or may not include measurement-based care.
Some KPNC patients may also have their mild-to-moderate depression or anxiety treated by their primary care physician if they prefer, and some KPNC medical centers have primary care-based collaborative psychiatric care programs.
Previous research has compared collaborative psychiatric care models to mental health managed within primary care. This is the first study to compare a collaborative model with specialty psychiatric care, Erickson-Ridout said.
The research is also unique in providing evidence about how these programs compare when care is provided virtually. While a lower proportion of KPNC patients are getting phone or video psychiatric care in the years since pandemic restrictions ended, a significant percentage still use virtual care.

“Since this virtual collaborative care program’s inception in April 2020, we have treated more than 37,000 patients with depressive and anxiety disorders,” said Lisa Fazzolari, DO, a TPMG psychiatrist and associate chair of psychiatry. “The telehealth platform allows for treatment to be easily accessible and convenient for large populations of patients. At KPNC, we have successfully implemented population management programs to treat patients with other chronic conditions such as diabetes, hypertension, and heart disease and are now applying this care approach to mental health.” Fazzolari noted that a new pilot program is testing collaborative care for depression and anxiety around the time of pregnancy.
The study was funded by The Permanente Medical Group Delivery Science and Applied Research program.
Additional co-authors were senior author Esti Iturralde, PhD, Constance M. Weisner, DrPH, and Mubarika Alavi, MS, of the Division of Research; Catherine Lee, PhD, formerly of the Division of Research; and Samuel J. Ridout, MD, PhD, and Sameer Awsare, MD, of The Permanente Medical Group; and Brooke Harris, PhD, of Kaiser Permanente Northern California.
# # #
About the Kaiser Permanente Division of Research
The Kaiser Permanente Division of Research conducts, publishes and disseminates epidemiologic and health services research to improve the health and medical care of Kaiser Permanente members and society at large. It seeks to understand the determinants of illness and well-being, and to improve the quality and cost-effectiveness of health care. Currently, DOR’s 600-plus staff is working on more than 450 epidemiological and health services research projects. For more information, visit divisionofresearch.kaiserpermanente.org or follow us @KPDOR.





This Post Has 0 Comments