Kaiser Permanente study showed that six blood pressure patterns can better stratify future risk of preeclampsia among ostensibly low- to moderate-risk patients
Routine blood pressure readings recorded in the first half of pregnancy can be divided into 6 distinct patterns that can effectively stratify patients by their risk of developing preeclampsia and gestational hypertension later in pregnancy, Kaiser Permanente researchers found.

The study, published July 12 in the Journal of the American Heart Association, showed that 6 pregnancy blood pressure trajectories seen within the first 20 weeks of pregnancy along with clinical, social, and behavioral risk factors can accurately predict and stratify risk of preeclampsia and gestational hypertension in low- to moderate-risk patients. Three of the early pregnancy blood pressure trajectories identified 74% of the patients who went on to develop preeclampsia later in their pregnancy.
“The prediction models accurately classified the patients with an increased risk for developing preeclampsia and gestational hypertension based on early blood pressure patterns several months before the onset of disease,” said lead author Erica P. Gunderson, PhD, MPH, a senior research scientist at the Kaiser Permanente Division of Research and a professor at the Kaiser Permanente Bernard J. Tyson School of Medicine.
“During a healthy pregnancy, blood pressure declines during the first half of pregnancy,” said Gunderson. “Our study found that patients who had moderately higher systolic blood pressure at the start of their pregnancy that didn’t decline as expected or had a normal blood pressure that increased through mid-pregnancy had the higher risk of developing early-onset or later-onset preeclampsia in the second half of pregnancy.”

The patients studied were considered to be low- to moderate-risk by current U.S. Preventive Services Task Force (USPSTF) risk criteria — a group for whom it has been challenging to identify individual risk of preeclampsia. Patients were relatively healthy, and did not have chronic hypertension, heart, kidney, or liver disease. About 1 in 10 patients in the study developed hypertensive disorders of pregnancy after 20 weeks: 0.4% developed early-onset preeclampsia (before 34 weeks of pregnancy), 4.3% developed later-onset preeclampsia, and 4.6% developed gestational hypertension.
Pregnant patients at higher risk for preeclampsia are followed more closely by their doctors and may also be treated with low-dose aspirin. The new study suggests that blood pressure trajectory groups may improve risk stratification and help health care providers identify patients who don’t appear to be at high risk in the first half of their pregnancy but actually are.
“Hypertensive disorders in pregnancy are leading causes of morbidity and mortality, particularly in people of color,” said Kari L. Carlson, MD, associate executive director for The Permanente Medical Group. “Identifying risk factors and then implementing a risk stratification program and treatment plan could have a huge impact for both the pregnant person and infant, dramatically reducing the chances of adverse outcomes.”
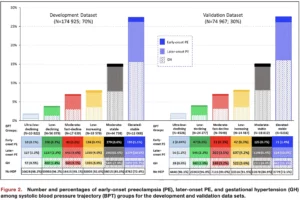 The large retrospective cohort study used routine clinical blood pressure measurements and clinical data from the electronic medical records of close to 250,000 healthy pregnant patients who gave birth to one child during a single pregnancy at a Kaiser Permanente Northern California hospital between 2009 and 2019. In a previous study, Gunderson’s team identified the 6 distinct blood pressure trajectories in a subset of about 175,000 of the patients.
The large retrospective cohort study used routine clinical blood pressure measurements and clinical data from the electronic medical records of close to 250,000 healthy pregnant patients who gave birth to one child during a single pregnancy at a Kaiser Permanente Northern California hospital between 2009 and 2019. In a previous study, Gunderson’s team identified the 6 distinct blood pressure trajectories in a subset of about 175,000 of the patients.
The new study used data from approximately 75,000 women not included in the prior study. It found that the model was able to predict and stratify risk of early onset and later onset preeclampsia and gestational hypertension based on the blood pressure trajectories and the additional clinical risk factors. The study also found the model worked equally well in the white, Black, Hispanic, and Asian patients included in the study.
“The use of a simple measure — blood pressure — that is available as part of clinical care to fine tune clinical risk assessment and identify those at highest risk could allow modification of care and the use of preventive therapies to the most appropriate patients,” said co-author James M. Roberts, MD, a professor of obstetrics, gynecology, and reproductive science at the University of Pittsburgh.
The researchers plan to develop an automated tool within the electronic health record system to identify patients in real time based on blood pressure patterns seen before 16 to 20 weeks of pregnancy. Care providers can then advise these patients of their higher risk for hypertensive disorders of pregnancy, offer available interventions, and provide additional monitoring.
“We wanted to find a way to stratify pregnant patients’ risk of preeclampsia and gestational hypertension so that we could improve health outcomes for moms and babies who might not be readily identified as being at high risk,” said Gunderson. “The wide availability of clinical blood pressure measurements from prenatal visits during the first 20 weeks of pregnancy makes it possible to potentially improve equity in care delivery, especially in under-resourced settings where expensive biomarkers and other tests are not accessible.”
The study was funded by the National Heart, Lung, and Blood Institute.
Co-authors include Baiyang Sun, MPH, Alan Go, MD, Mai N. Nguyen-Huynh, MD, MAS, Wei Tao, MS, and Stacey E. Alexeeff, PhD, of the Division of Research, and Nancy Goler, MD, and Mara Greenberg, MD, of The Permanente Medical Group.
# # #
About the Kaiser Permanente Division of Research
The Kaiser Permanente Division of Research conducts, publishes and disseminates epidemiologic and health services research to improve the health and medical care of Kaiser Permanente members and society at large. It seeks to understand the determinants of illness and well-being, and to improve the quality and cost-effectiveness of health care. Currently, DOR’s 600-plus staff is working on more than 450 epidemiological and health services research projects. For more information, visit divisionofresearch.kaiserpermanente.org or follow us @KPDOR.





This Post Has 0 Comments