Long-term review at Kaiser Permanente Northern California finds no differences in reinterventions by race or ethnicity
Uterine fibroids are a common, non-cancerous condition that can be treated using several different methods that preserve the uterus. A long-term review of Kaiser Permanente Northern California (KPNC) patients finds varying rates of follow-up procedures.
Patients who had myomectomy, which is surgical removal of the fibroid, had the lowest rate of follow-up procedures at 7 years compared with those who had other methods of treatment.

The analysis, published in Obstetrics & Gynecology, studied a larger number of patients for a longer period of time than previous studies, said lead author Susanna Mitro, PhD, a research scientist with the Kaiser Permanente Division of Research (DOR).
“We had a unique opportunity to examine a large number of patients to do a good comparison,” Mitro said. “Having this information about long-term follow-up is a big step forward in understanding what happened to people who chose one of these treatment options versus the others.”
While benign, uterine fibroids can grow large and numerous, causing pain, interference with fertility, and other problems. They are the most common non-cancerous reason women have hysterectomies — the surgical removal of the uterus.
Fibroids can be treated with hysterectomy, but many patients prefer to preserve their uterus for future pregnancy or other reasons. The 4 main uterine-preserving procedures all have some rate of re-intervention because of fibroid recurrence.
The researchers studied 10,324 patients aged 18 to 50 who had a first uterine-preserving procedure between 2009 and 2021 and followed their progress until a second procedure.

After 7 years, myomectomy had the lowest reintervention rate of 20.6%, followed by uterine artery embolization (26%), endometrial ablation (35.5%), and hysteroscopic myomectomy (37%). Embolization involves blocking the blood supply to the uterus; ablation removes the uterus lining; hysteroscopic fibroid removal is a minimally invasive procedure.
Reintervention rates varied by patient age, with younger patients having higher rates of reintervention after embolization, ablation, and minimally invasive surgery.
The median period for a follow-up procedure was 3.8 years. Nearly two-thirds of the follow-up procedures were hysterectomies.
“This study really better defines what is happening to our patients and is helpful in counseling patients when they are considering interventions,” said co-author Eve Zaritsky, MD, a minimally invasive gynecologic surgeon with The Permanente Medical Group.
No disparities found
Zaritsky said it is encouraging that the analysis did not find a difference in reintervention rates by race or ethnicity, particularly because fibroids affect Black women disproportionately. “When I saw these findings, I was delighted to see that these reintervention procedures were distributed at KPNC equally among patients of all racial and ethnic backgrounds,” she said.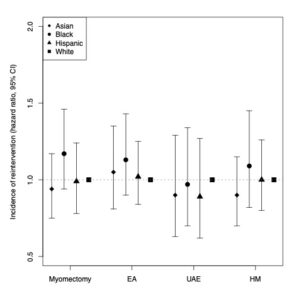
Prior research has found no differences by race in the treatment of benign gynecologic conditions at KPNC. A 2019 study led by Zaritsky reported that that nearly all patients were offered and tried at least one type of alternative treatment before hysterectomy. Another of her studies observed that KPNC had eliminated a racial disparity in providing the preferred minimally invasive hysterectomy over open abdominal procedures.
The findings may guide clinicians in their recommendations of primary and secondary procedures for patients with fibroids, Zaritsky said. “Given the results of our 7-year longitudinal study, our clinicians can better counsel our patients about interventions,” she said.
At the same time, she said, fibroid quantity and growth are highly variable from patient to patient, so the choice of procedure and any follow-up are patient centered.
“I am pleased to see the valuable findings from this important study that will inform patient decisions for how to treat their fibroids,” said senior author Monique Hedderson, PhD, a DOR research scientist. “Benign gynecologic conditions such as fibroids affect a large number of women, but treatments have historically been understudied.”
The study was funded by the National Institute of Arthritis and Musculoskeletal and Skin Diseases.
Additional co-authors were Fei Zhu, MS, and Catherine Lee, PhD, of the Division of Research; L. Elaine Waetjen, MD, of the University of California, Davis; and Lauren A. Wise, ScD, of Boston University.
# # #
About the Kaiser Permanente Division of Research
The Kaiser Permanente Division of Research conducts, publishes and disseminates epidemiologic and health services research to improve the health and medical care of Kaiser Permanente members and society at large. It seeks to understand the determinants of illness and well-being, and to improve the quality and cost-effectiveness of health care. Currently, DOR’s 600-plus staff is working on more than 450 epidemiological and health services research projects. For more information, visit divisionofresearch.kaiserpermanente.org or follow us @KPDOR.





This Post Has 0 Comments