Large Kaiser Permanente study will lead to better management for patients with the common heart valve condition
The diagnosed severity of aortic stenosis strongly correlates with clinical outcomes, new Kaiser Permanente research shows. But the study also suggests that fine-tuning assessments of the patients with moderate aortic stenosis could help improve outcomes and better determine which patients might benefit from surgery.
The study, published in the American Heart Journal, found that patients diagnosed with moderate aortic stenosis have outcomes most similar to those categorized by physicians with mild aortic stenosis while only those with moderate-to-severe aortic stenosis had outcomes similar to those with severe aortic stenosis.

“Moderate aortic stenosis represents a wide spectrum of disease,” said Matthew D. Solomon, MD, PhD, a physician researcher at the Kaiser Permanente Division of Research and a cardiologist at The Permanente Medical Group. “Despite controversy in the field about the prognosis for these patients, our results show that moderate aortic stenosis patients have a different trajectory than those with severe aortic stenosis, and that they can be safely followed with close surveillance.”
Aortic stenosis is a condition in which the heart’s aortic valve becomes stiff and can’t fully open. It is the most common valvular heart disease condition, affecting 1 in 8 people aged 75 and over. Severe aortic stenosis, when accompanied by symptoms, is typically treated with surgery to replace the aortic valve. Some recent studies have suggested that moderate aortic stenosis disease may be as deadly as severe aortic stenosis, and that these patients might benefit from surgery. The Kaiser Permanente study is the largest to date to look at patients’ prognosis based on the severity of their disease.
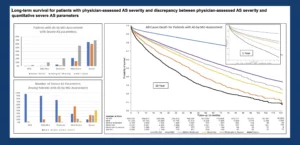 The new study included nearly 547,000 Kaiser Permanente Northern California patients who had an echocardiogram between 2008 and 2018 to determine if they had aortic stenosis. An echocardiogram is a type of ultrasound test that can show how well blood is moving through the heart and its valves. Close to 50,000 patients were identified as having mild, mild-to-moderate, moderate, moderate-severe, or severe aortic stenosis. The research team analyzed associations between the physician assessments and the patients’ clinical outcomes — hospitalization for heart problems, surgery to replace the aortic valve, or death.
The new study included nearly 547,000 Kaiser Permanente Northern California patients who had an echocardiogram between 2008 and 2018 to determine if they had aortic stenosis. An echocardiogram is a type of ultrasound test that can show how well blood is moving through the heart and its valves. Close to 50,000 patients were identified as having mild, mild-to-moderate, moderate, moderate-severe, or severe aortic stenosis. The research team analyzed associations between the physician assessments and the patients’ clinical outcomes — hospitalization for heart problems, surgery to replace the aortic valve, or death.
“We took on the necessary and difficult task of building a research-grade database from our 1,000,000 echocardiograms performed at Kaiser Permanente Northern California over the past decade to be able to answer critical questions in the field,” said Solomon. “Five years ago, we wouldn’t have been able to do this research. Now, we have the largest aortic stenosis dataset in the world and are using our findings to implement a comprehensive population management program for Kaiser Permanente patients with aortic stenosis.”
. . . we are using our findings to implement a comprehensive population management program for Kaiser Permanente patients with aortic stenosis.
— Matthew Solomon, MD, PhD
“This very small valve opening was sometimes seen in patients who had aortic stenosis classified as moderate or moderate-severe based on other measurements seen on the echocardiogram,” said Solomon. “We learned that aortic valve area is the key indicator of aortic stenosis severity and that a low aortic valve area should alert physicians that the severity of a patient’s disease may be worse than other echocardiographic parameters suggest.”

For decades, open heart surgery was the only treatment option for severe aortic stenosis. Today, most patients are treated with a minimally invasive procedure called a transcatheter aortic valve replacement (TAVR). The procedure requires an interventional cardiologist to insert a thin tube into a blood vessel in the groin or chest, guide it to the heart, and then use miniature tools that fit inside the tube to put a new valve in place. The procedure takes significantly less time than open heart surgery, and recovery is much faster — but it still carries potential risks.
“Kaiser Permanente is a leader in providing cutting-edge treatments in patients with valve disease,” said co-author Femi Philip, MD, an interventional cardiologist with The Permanente Medical Group. “We are one of the largest TAVR centers in the U.S., and we can use these data to better identify severe aortic stenosis patients to ensure they are seen by our specialized heart teams and evaluated for this life-saving treatment.”
To better understand whether earlier treatment will benefit aortic stenosis patients, Kaiser Permanente Northern California is one of more than 70 hospitals throughout the world currently enrolling patients with moderate aortic stenosis in a large randomized controlled trial to compare benefits and risks of TAVR surgery with clinical surveillance.

“This unique study linked together detailed clinical information from echocardiography reports and other longitudinal electronic health record data on a large scale to provide new insights for providers and patients on future outcomes of aortic stenosis within a contemporary, sociodemographically diverse population,” said senior author Alan Go, MD, associate director at the Kaiser Permanente Division of Research overseeing cardiovascular and metabolic conditions research.
Solomon says this is the first of many studies that the new database will make possible. “We are now in a position to study outcomes for other major valvular heart conditions, such as mitral regurgitation. These studies will all have the same goal: using data we can only gather at Kaiser Permanente to improve care for patients nationwide.”
The study was funded by The Permanente Medical Group Delivery Science and Applied Research Program.
Coauthors include Grace Tabada, MPH, Sue Hee Sung, MPH, Amanda Allen, BA, Andrew Ambrosy, MD, and Catherine Lee, PhD, of the Division of Research; Jacob Mishell, MD, Andrew N. Rassi, MD, Edward McNulty, MD, David C. Lange, MD, Jonathan G. Zaroff, MD, and Ashok Krishnaswami, MD, of The Permanente Medical Group; Anthony DeMaria, MD, of the University of California, San Diego; and Rick Nishimura, MD, of The Mayo Clinic.
# # #
About the Kaiser Permanente Division of Research
The Kaiser Permanente Division of Research conducts, publishes and disseminates epidemiologic and health services research to improve the health and medical care of Kaiser Permanente members and society at large. It seeks to understand the determinants of illness and well-being, and to improve the quality and cost-effectiveness of health care. Currently, DOR’s 600-plus staff is working on more than 450 epidemiological and health services research projects. For more information, visit divisionofresearch.kaiserpermanente.org or follow us @KPDOR.





Comments (0)