Kaiser Permanente study finds promise in ‘food as medicine’ delivery for some — but not all — patients with chronic conditions
Healthy eating patterns are key to reducing risk for common health problems and maintaining a healthy weight. Providing lower-sodium, heart-healthy meals to people with chronic health problems is a popular approach to integrating nutrition into medical care. A Kaiser Permanente study suggests these medically tailored meals may benefit recently hospitalized patients with heart failure, adding to the growing body of research on food as medicine.

“People with certain chronic disease often are given guidelines for healthy meals, but they may not be financially or physically able to prepare them,” said first author Alan Go, MD, a research scientist at the Kaiser Permanente Northern California Division of Research. “We had hoped that delivering these meals tailored to the specific dietary needs of people with heart failure, diabetes, and chronic kidney disease would improve clinical outcomes. What we found was that they may benefit people with heart failure, but we need to do more research to establish how we can best use food as medicine in different nutrition-sensitive conditions.”
The study, published in Medical Care, included 1,977 adults previously diagnosed with heart failure, diabetes, or chronic kidney disease who were discharged from 5 Kaiser Permanente Northern California (KPNC) hospitals between April 2020 and June 2021. Half of the study participants were randomly selected to have medically tailored meals delivered to their homes for up to 10 weeks; the other half received usual care. In addition, half of the people who received the special meals also were offered 3 sessions of nutrition counseling, delivered virtually.
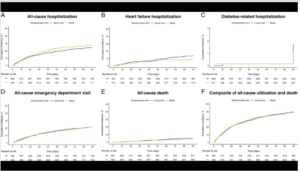
The study found that the adults who received the meals — including those who received nutritional counseling — were not less likely to be hospitalized again within 90 days than those who received usual care. In addition, emergency department visits and diabetes-related hospitalizations were similar for both groups. However, the patients who received meals were slightly less likely to die over the next 90 days than the patients who received usual care, and they had fewer hospitalizations for heart failure.
“As a doctor and a chef, I believe that if we don’t address what people are eating, and help make sure they are getting good nourishment, we are missing a crucial step to improving health,” said Linda Shiue, MD, a specialist in internal medicine and the director of culinary medicine for Kaiser Permanente San Francisco. “Randomized controlled trials like this one are the gold standard, but with nutrition studies, there may be benefits we miss because we aren’t accounting for what else people were eating or if they ate the meals they received.”

Increased attention to hunger, food insecurity, and food deserts — along with the growing number of people in the U.S. with an obesity-related chronic disease — have prompted communities to find ways to get fresh produce and healthy meals into low-income communities or to housebound adults. But few studies have evaluated whether these new or ongoing efforts successfully reduce risk for — or help people already diagnosed with — a chronic disease.
In 2020, Kaiser Permanente launched 3 studies in Kaiser Permanente regions in Northern California, Colorado, and the Northwest to investigate the benefits of home-delivered medically tailored meals for patients with chronic conditions such as heart failure, diabetes, and kidney disease. The new study, called KP NOURISH (Kaiser Permanente Evaluation of Medically Tailored Meals in Adults with Chronic Medical Conditions at High Readmission Risk), is the first to report its findings.
KP NOURISH provided 1 large medically tailored meal per day to the study participant and to other eligible household members. Among the study participants, 32% had heart failure, 69% had diabetes and 45% had chronic kidney disease (some people had more than one illness).
All the meals met standards established by the Food is Medicine coalition, and typically followed the DASH (Dietary Approaches to Stop Hypertension) eating plan: a lower-salt, low-fat diet comprised of lean proteins, vegetables, whole grains, and healthy fats.
The potential benefits may not have been fully realized because only about half of the 993 participants who initially received the medically tailored meals agreed to receive them for the full 10 weeks.

Medi-Cal health plans recently launched a 5-year program that will cover up to 3 home-delivered, medically tailored meals per day for up to 12 weeks, or longer if medically necessary, to people with chronic conditions who have been discharged from a hospital. By providing these meals, Medi-Cal hopes these patients will see nutritional benefits that help keep them out of the hospital or emergency room and improve their overall health.
“Food as medicine programs are being accelerated throughout the nation,” said Pam Schwartz, MPH, the executive director of Community Health for Kaiser Permanente. “Kaiser Permanente is proud to be part of the growing movement in health care and to invest in the research that will allow us to learn what works best and under what conditions for the people with chronic health issues who have the potential to benefit from these programs.”
The study was supported by Kaiser Permanente.
Co-authors include Thida C. Tan, MPH, Kate M. Horiuchi, BS, Andrew P. Ambrosy, MD, Keane K. Lee, MD, MS, Joan C. Lo, MS, MD, and Rishi V. Parikh, MPH, of the Division of Research; Denise Laws, RN, DP, Jena Joy, MD, and Benjamin L. Maring, MD, MPH, of The Permanente Medical Group; Cathryn Couch, MBA, of the Ceres Community Project; and Paul Hepfer, MS, of Project Open Hand, for the KP NOURISH Study Investigators.
# # #
About the Kaiser Permanente Division of Research
The Kaiser Permanente Division of Research conducts, publishes and disseminates epidemiologic and health services research to improve the health and medical care of Kaiser Permanente members and society at large. It seeks to understand the determinants of illness and well-being, and to improve the quality and cost-effectiveness of health care. Currently, DOR’s 600-plus staff is working on more than 450 epidemiological and health services research projects. For more information, visit divisionofresearch.kaiserpermanente.org or follow us @KPDOR.





Comments (0)